Posterior Malleolus Component Reduced in a Near Anatomic Fashion
Original Editor - Andrea Nees as office of the Vrije Universiteit Brussel Evidence-Based Practise Project
Top Contributors - George Prudden, Andrea Nees, Kim Jackson, Eta Frida, Rachael Lowe, Admin, WikiSysop, Scott Cornish, Luna Antonis, Wanda van Niekerk, Evan Thomas, Karen Wilson, Haddad Yousri and Claire Knott
Clarification [edit | edit source]
A fracture is an interruption of the continuity of bone, this folio volition discuss ankle and foot fractures and the function that physiotherapists play in the rehabiliation of such injuries. Fractures of the ankle articulation are common amongst adults. Kannus et al. written report an incidence of upwards to 174 cases per 100 000 persons per twelvemonth in a Finish population.[1] Fractures of the pes are less common.
Fractures of the talocrural joint [edit | edit source]
Ankle fractures are virtually commonly diagnosised through clinical examination and 10-ray. Ottawa rules provide clinicians with a tool to decide whether the joint should exist imaged or not. Several classifications exist and are used to decide severity of injury and management. Examples are Danis-Weber that identifies level of injury and Lauge-Hansen and uses machinery of the injury.
Complications include reduced range of motion at the ankle and foot joint as a outcome of peri-articular and intra-articular adhesions or disruption of articular surfaces. Disruption to articular surfaces may lead to development of osteoarthritis.
Fractures without deportation can be treated with a below knee bandage that may be applied for 3-6 weeks. If displaced, a surgeon should reduce the fragments to there normal anatomical position of the articulation. If this cannot be achieved past manipulation and plaster cast and so an private may take to undergo an open reduction with internal fixation (ORIF) followed by immobilisation in a plaster cast.[two]
- Potts Fracture
- Avulsion Fractures
Fractures in the pes [edit | edit source]
The bony anatomy of the pes means that at that place are a variety of fractures. Fractures of the calcaneum often occur every bit a upshot of a fall from height. Such fractures tin exist very painful and may be accompanied by vertebral fractures. The phalanges and metatarsals are commonly injuried by a heavy object falling onto the foot. These fractures exercise not require reduction or immobilisation. Stress fractures of the metatarsals are known as a 'March' fracture. These are caused by repeated trauma from pronlonged walking.[2]
- Calcaneal Fractures
- Chopart fracture-dislocation
- Metatarsal Fractures
Stress Fractures [edit | edit source]
Stress fractures occur in bones that undergo mechanical fatigue.[3] They are a issue of exceeding repetitive submaximal loads, which creates an imbalance between bone resorption and bone formation.[4] The fractures usually brainstorm in locations of slap-up stress; this is called "cleft initiation".[4] If this microscopic crack is non able to heal and is subjected to farther loading, the microdamage will increase and the scissure volition overstate. This increase in harm can cause the bone to break on a macroscopic level.[4]
- Leg and Fott Stres Fractures
Clinically Relevant Anatomy [edit | edit source]
The ankle articulation [edit | edit source]
The talocrural joint joint also known as talocrural joint is fabricated upwards of three bony structures: the distal ends of the tibia (shinbone) and fibula and the talus. The tibia and fibula take specific parts that make up the ankle:
- Medial malleolus - inside part of the tibia
- Posterior malleolus - back part of the tibia
- Lateral malleolus – end of the fibula
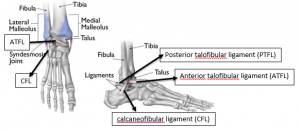
The tibia and fibula form the talocrural joint articulation with structure and stability provided by connective tissues:
- Interosseous membrane
- Anterior, posterior, and transverse tibiofibular ligaments
The collateral ligaments stabilize the articulation against abduction and adduction forces. Laterally, the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL), and, medially, the wide fan of the deltoid ligament and the plantar calcaneonavicular ligament, whose medial edge is blended with the forepart of the deltoid ligament.[five]
The foot [edit | edit source]
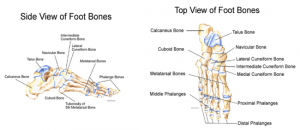
The human foot contains 26 bones. The foot is divided into 3 main parts: hindfoot, midfoot and forefoot.
- Hindfoot is composed of 2 basic, calcaneus and talus. They form the subtalar joint
- Midfoot is made upwardly of 5 bones, navicular, cuboid and 3 cuneiforms (medial, intermediate and lateral). The bones are continued to the forefoot and the hindfoot past muscles and the plantar fascia (arch ligament).
- Forefoot is consists of 19 bones, which are 5 metatarsals, 14 phalanges.
The Chopart articulation is the connection between the hindfoot to the midfoot involving the 'talonavicular joint' and the 'calcaneocuboid joint'; the Lisfranc joint connects the forefoot to the midfoot.
Epidemiology /Etiology [edit | edit source]
Ankle fracture is caused by traumas such as falls, twisting injuries and sports-related injuries[half-dozen] [vi], and therefore it does not only occur in the older, but also in the young and active population.
There are a number of take a chance factors associated with an increased hazard of sustaining foot and ankle fractures including smoking, diabetes, obesity, previous falls and/or fractures, very high or low levels of physical activity, and low bone mineral density (BMD). For older individuals over an age of 50, additional gamble factors include female gender, comorbidities and multiple medications.
The higher level of activeness in younger males, particularly in risk taking and sports activities, might explain the high rates of ankle and foot fractures in this historic period group. Younger female, under the age of 50, less agile than males, yet they accept a higher tendency to fall, afterwards in life which coincides with postmenopausal bone loss, resulting in an increase in fracture risk.[vii]
Characteristics/Clinical Presentation [edit | edit source]
- Difficulties or fifty-fifty inability to walk or load the ankle. (information technology is possible to walk with less astringent breaks, so never rely on walking every bit a test of whether a os has been fractured.
- Hurting
- Swelling
- Bruising (soon after the injury).
- Difference in appearance.
- Observable differences compared to the unaffected side
When an ankle has been cleaved, there is non only structural impairment to the skeletal construction, but also to the ligament tissue (deltoid ligament and the anterior and posterior tibiofibular ligaments) and possibly nervous and musculoskeletal tissue effectually the talocrural joint circuitous. This can result in impaired rest chapters, reduced joint position sense, slowed nerve conduction, velocity, impaired cutaneous sensation and decreased dorsal extension range of motion[six]
Fracture Classifications [edit | edit source]
Ankle fractures tin can be classified according to either the AO/OTA, Danis-Weber or Lauge-Hansen classification system.
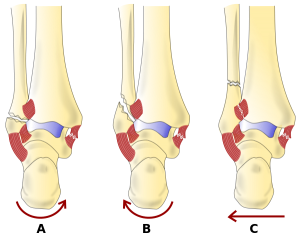
The Lauge-Hansen nomenclature is based on a rotational mechanism of injury. At that place are iv categories and 13 subgroups of ankle fractures detailed in the table beneath.
| Categories | Stage (subgroups) |
| Supination external rotation (SER) | one. Injury of the inductive junior tibiofibular ligament 2. Oblique/spiral fracture of the distal fibula 3. Injury of the posterior inferior tibiofibular ligament or avulsion of the posterior malleolus iv. Medial malleolus fracture or injury to the deltoid ligament |
| Supination adduction (SA) | 1. Transverse fracture of the distal fibula 2. Vertical fracture of the medial malleolus |
| Pronation external rotation (PER) | ane. Medial malleolus fracture or injury to the deltoid ligament 2. Injury of the anterior inferior tibiofibular ligament three. Oblique/screw fracture of the fibula proximal to the tibial plafond 4. Injury of the posterior junior tibiofibular ligament or avulsion of the posterior malleolus |
| Pronation abduction (PA) | 1. Medial malleolus fracture or injury to the deltoid ligament ii. Injury of the anterior junior tibiofibular ligament 3. Transverse or comminuted fracture of the fibula proximal to the tibial plafond |
The Danis-Weber classification is based on radiographic criteria. It took into consideration the position of the distal fibular fracture in relation to the syndesmosis of the ankle joint. Iii categories were created:
- Type A fracture: below the level of the tibial plafond (syndesmosis) and may be associated with oblique or vertical medial malleolar fractures
- Type B fractures: at the level of the tibial plafond (syndesmosis) and extend proximally in an oblique fashion
- Type C fractures: proximal to the level of the tibial plafond and oftentimes take an associated syndesmotic injury. It can be associated with medial malleolus fractures or injury to the deltoid ligament.[5] [eight]
The AO and Lauge-Hansen nomenclature systems are widely used in the clinical diagnosis of ankle injuries. The AO classification system is simple to understand, and it emphasizes the coordinating role of the fibula and syndesmosis of the ankle joint. The Lauge-Hansen classification system emphasizes the different stages of pathological harm in addition to the fracture pattern, and information technology insists on the understanding of damage to the talocrural joint ligament system. Information technology can provide an extensive cess of ankle injuries.
Compared to Lauge-Hansen classification, AO classification system is more reliable and reproducible and thus has more than value in clinical practise, than the Lauge-Hansen nomenclature system. Despite this, the Lauge-Hansen classification system stands equally the basis for understanding the mechanics of ankle fractures.[9]
AO classification/OTA organization classifies all long bone fractures with a systematic approach, based on location, topography, and extent of bony lesion. It is based on radiographic criteria and incorporates the machinery of injury. The fractures are classified equally infrasyndesmotic, transsyndesmotic and suprasyndesmotic with farther subcategories based on the presence or absence of medial or posterior malleolar injuries.
The tabular array below compares the Danis-Weber, Lauge-Hansen, and AO/OTA classification systems.
| Fibular fracture location | Danis-Weber classification | Lauge-Hansen classification SAD I, II | AO/OTA classification of tibial malleolar fractures |
| Infrasyndesmotic | Type A | Sad I, 2 | 44-A1 (isolated lateral) 44-A2 (lateral and medial) 44-A3 (lateral, medial, and posterior) |
| Transsyndesmotic | Type B | SER I, II, III, IV | 44-B1 (isolated lateral) 44-B2 (lateral and medial) 44-B3 (lateral, medial, and Volkmann'southward fracture) |
| Suprasyndesmotic | Type C | PER I, Two, III, IV PA I, Ii, III | 44-C1 (simple diaphyseal) 44-C2 (multifragmentary) 44-C3 (proximal |
OTA = Orthopaedic Trauma Association; Lamentable = supination adduction; SER = supination external rotation; PER = pronation external rotation; PA = pronation abduction.[8]
Differential Diagnosis [edit | edit source]
- Rheumatoid Arthritis
- Gout and Pseudogout
- Ankle Dislocation
- Ankle Impingement
- Compartment Syndrome of the Foot
- Deep Venous Thrombosis
- Peroneal Tendinopathy
- Sinus Tarsi Syndrome
- Ankle ligament sprains.
The clinical presentation of some subtle fractures of the ankle tin can be similar to that of ankle sprains. This similarity makes that talocrural joint fracture is often mistaken as ankle sprain. These injuries are quite different and need an accurate and early on diagnosis.[10]
Diagnostic Procedures [edit | edit source]
Ottawa rules [edit | edit source]
Ankle Ten-ray is only required if there is any pain in the malleolar zone and whatever one of the post-obit:
- Bone tenderness forth the distal 6 cm of the posterior edge of the tibia or tip of the medial malleolus, OR
- Os tenderness along the distal 6 cm of the posterior edge of the fibula or tip of the lateral malleolus, OR
- An inability to carry weight both immediately and in the emergency department for four steps.
Additionally, the Ottawa ankle rules bespeak whether a foot X-ray series is required. It states that it is indicated if there is any pain in the midfoot zone and any one of the following:
- Os tenderness at the base of operations of the 5th metatarsal (for foot injuries), OR
- Bone tenderness at the navicular bone (for foot injuries), OR
- An inability to behave weight both immediately and in the emergency section for four steps.
Ankle fractures are initially evaluated by physical examination and so by x-ray.[v]
To reduce the apply of 10-rays, an intrasound device can be used to detect malleolar fractures even though it cannot be relied upon solitary due to an 85% sensitivity and 52% sensitivity.[11]
Ultrasound had good sensitivity and specificity for diagnosing 5th metatarsal, lateral and medial malleolus fractures in patients with foot and/or talocrural joint sprains. However, sensitivity and specificity of ultrasound for navicular fractures were low.[8]
Imaging [edit | edit source]
Outcomes Measures [edit | edit source]
- SF-36 includes 8 categories: Physical functioning, Physical role, Bodily pain, General health, Vitality, Social functioning, Emotional role and Mental health)[12]
- Kerr-Atkins score for hurting and function afterward calcaneal fracture leading to a best score of 100points.[6]
- EuroQol (EQ-5D) to measure the Quality of life and general health status[half dozen]
- American Orthopaedic Foot and Ankle Gild score based on 9 items: hurting, action and functional limitations, walking altitude, difficulties with dissimilar terrains, gait abnormality, sagittal range of motion at the ankle and range of motion at the subtalar joint, stability, and alignment[13]
- Olerud-Molander Ankle Score (OMAS), is an ordinal rating scale from 0 points (totally impaired office) to 100 points (completely unimpaired function) related to ix different items given dissimilar points: pain, stiffness, swelling, stair climbing, running, jumping, squatting, supports and piece of work/activity level.[fourteen]
- FAOS is likewise a self-administered patient questionnaire and consists of 42 items divided into 5 subscales: hurting, other symptoms, function in daily living (ADL), part in sport + recreation + human foot and ankle-related quality of life.[fourteen]
- Global self-rated ankle (GSRF) to evaluate their present talocrural joint function[xiv]
- The American Orthopaedic Foot and Ankle Society Hindfoot score (AOFAS) score contains 3 components: pain (40 points), role and alignment on a scale of 0- 100 points, 100 best possible score[7]
- Foot Function Index (FFI) consists of 23 questions to measure the impact of human foot pathology on function in terms of hurting, disability and brake of activity. The lower the score, the better result[7]
Medical Direction [edit | edit source]
Most patients with a malleolus fracture require six weeks of immobilisation. Patients with an initially non-displaced fracture or who were treated surgically will generally require 4 weeks of non-weight bearing in a brusk-leg bandage or removable walking kicking, followed by 2 weeks in a walking cast or kicking. The removable boot will allow for earlier range-of-motion exercises.
Surgery is needed for many types of ankle fractures. While not always necessary, surgery for talocrural joint fractures is non uncommon. The need for surgery depends on the appearance of the ankle joint on X-ray and the type of ankle fracture.
The goals of surgery are always the shine anatomical reconstruction of the joint surface and the protection of the injured ligamentous structures to enable early on postoperative functional therapy of the joint. Adequate reduction with congruency of the articulation has been reported as i of the most important indications of a proficient end result. Inadequate reduction may lead to osteoarthritis.
The timing of definitive surgical treatment depends mainly on the soft-tissue findings, is possible only if the soft tissues are non critically vulnerable (few hours afterwards the trauma). And so the demand for surgery depends on the appearance of the talocrural joint joint on X-ray and the blazon of ankle fracture.
While non always necessary, surgery for ankle fractures can be done with 3 kinds of metal plate and multiple screws: one-third tubular plate; locking pinch (LCP) metaphyseal plate for lateral malleolar fracture and Weber B fracture; LCP distal fibula plate Weber A fracture and Weber B fracture.[5] [xv]

Types of plates- from left to correct: conventional one-3rd tubular plate; a LCP metaphyseal plate; a LCP distal fibula plate
Physical Therapy Management [edit | edit source]
Fractures that are stable with non-displaced or only slightly displaced fragments tin can be treated conservatively. Type A fractures exercise not demand to be immobilised in a bandage, only can rather be treated like external ligament ruptures in a stabilising ankle orthosis for early on function with pain-adapted total weight-begetting.[5](Level of Evidence 5)

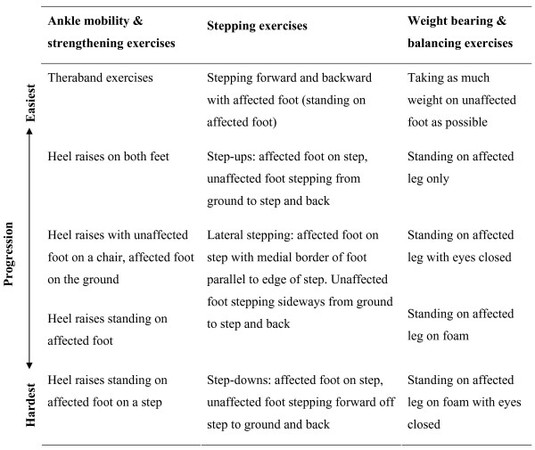
Passive articulation mobilization
More pregnant fractures are immobilised and require a rehabilitation programme after bandage removal. Programs should exist patient centred and accept into consideration patient goals and aspirations. Programs tend to include talocrural joint mobility, strengthening do, weight bearing and balancing exercise. Physiotherapists should empower the patient with home exercises and provide pedagogy and advice.[6]
Patients ofttimes complain of difficulties with activities involving the lower limb, such every bit stair climbing, walking and reduced participation in work and recreation. Impairments can be hurting, swelling, stiffness, muscle atrophy and decreased muscle torque[nine](Level of Bear witness 4), impaired ankle mobility, impaired balance chapters and increased ankle circumference[vi](Level of Bear witness 2A) at the ankle later on cast removal.
Passive articulation mobilisation can be used to piece of work on the issues of pain and joint stiffness, in order to allow an before render to activities. For this technique, the physiotherapist manually glides the articular surfaces of a articulation to produce oscillatory movements.[16] (Level of Bear witness 1A)Manual techniques should be complimentary to a program that includes agile exercise.
Strength-preparation may be beneficial after fracture and should be considered as an important rehabilitation option by physiotherapy. Because strength loss is one of the most common complications by a foot or ankle fracture.[17] (Level od Bear witness 1A)
Key Research [edit | edit source]
- Fractures of the Ankle Joint: Investigation and Treatment Options.[v]
- Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review.[18]
Resources [edit | edit source]
- Orthopaedic Surgery ucsf. Ankle Concrete Examination. http://orthosurg.ucsf.edu/oti/patient-care/divisions/sports-medicine/physical-test-info/ankle-concrete-exam/ (accessed 24 Aug 2014).
References [edit | edit source]
- ↑ Kannus P, Palvanen M, Niemi S, Parkkari J, Jrvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: finnish statistics during 1970–2000 and projections for the hereafter. Bone. 2002;31(iii):430-433.
- ↑ 2.0 2.one Tidy N, Porter S. Tidy'south physiotherapy. 13th ed. Edinburgh: Elsevier; 2013.
- ↑ Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of running speed on a probabilistic stress fracture model. Clinical Biomechanics. 2010;25:372-377.
- ↑ 4.0 iv.i 4.two Maffulli N, Longo UG, Denaro V. Femoral Cervix Stress Fractures. Operative Techniques in Sports Medicine. 2009;17:ninety-93.
- ↑ 5.0 five.1 5.two 5.iii 5.iv v.5 Goost H et al. Fractures of the Ankle Joint: Investigation and Treatment Options. Dtsch Arztebl Int. 2014; 111(21): 377–388.fckLRhttp://www.ncbi.nlm.nih.gov/pmc/manufactures/PMC4075279/ (
- ↑ 6.0 6.i half-dozen.2 6.3 half dozen.4 vi.5 6.half dozen Peter J. Daly et al. Epidemiology of ankle fractures in Rochester, Minnesota, Acta Orthopaedica Scandinavica. 1987; 58:5, 539-544 (Level of testify 2A)
- ↑ 7.0 7.i 7.two Holloway KL et al. Foot and Ankle Fracture Incidence in South-Eastern Australia: An Epidemiological Study. Clin Res Pes Ankle 2014, 2:iv
- ↑ 8.0 8.1 8.two Jason P. Tartaglione et al. Classifications in Cursory: Lauge-Hansen Classification of Talocrural joint Fractures. Clin Orthop Relat Res (2015) 473:3323–3328
- ↑ ix.0 9.1 Meng-chen Y et al. Evaluating the Reliability and Reproducibility of the AO and Lauge-Hansen Nomenclature Systems for Ankle Injuries. Orthopedics. 2015; 38(7): 626-30. (Level of evidence 4)
- ↑ Judd DB, Kim DH. Foot fractures frequently misdiagnosed every bit talocrural joint sprains. Am Fam Physician. 2002; 66(5):785-94.
- ↑ Dancocks A et al. A pilot study to appraise the sensitivity and specificity of an intrasound device in the diagnosis of ankle fractures. J Accid Emerg Med. 1997; 14(4): 230–232.
- ↑ Westphal T, Piatek South, Halm JP, Schubert S, Winckler Southward. Outcome of surgically treated intraarticular calcaneus fractures - SF-36 compared with AOFAS and MFS. Acta Orthopaedica Scandinavica. 2004; 75(6): 750-755.
- ↑ Van Schie-Van der Weert EM, Van Lieshout, EMM, De Vries MR, Van der Elst 1000, Schepers T. Determinants of issue in operatively and not-operatively treated Weber-B ankle fractures. Arch Orthop Trauma Surg. 2012 February; 132(two): 257–263.
- ↑ fourteen.0 14.1 fourteen.2 Nilsson GM, Eneroth K, Ekdahl CS. The Swedish version of OMAS is a reliable and valid outcome measure for patients with talocrural joint fractures. BMC Musculoskelet Disord. 2013; 14: 109.
- ↑ Huang Z et al. Comparison of three plate system for lateral malleolar fixation. BMC Musculoskelet Disord. 2014; 15: 360. (2B).fckLRhttp://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223732/
- ↑ Lin C CH, Moseley AM, Refshauge KM, Haas M, Herbert RD. Effectiveness of articulation mobilisation after cast immobilisation for ankle fracture: a protocol for a randomised controlled trial. BMC Musculoskeletal Disorders 2006;7:46 (Level of evidence1A)
- ↑ Murdoch A, Taylor N, Dodd M. Physical therapist should consider including training as part of fracture rehabilitation. Physical Therapy Reviews (2004) Mar(9) 1 51 – 59
- ↑ Bachmann LM et al. Accuracy of Ottawa ankle rules to exclude fractures of the talocrural joint and mid-human foot: systematic review. BMJ 2003; 236:417
0 Response to "Posterior Malleolus Component Reduced in a Near Anatomic Fashion"
Post a Comment